Portfolio Pains
This week I thought I'd delve into the world of Surgeons' Portfolios @JCST_Surgery. Whether you call it Eye Ess Sea Pee, ICECAP or (if you're getting close to the ARCP) something more fruity and Anglo-Saxon, it is here to stay and if steered correctly provides magnificent evidence of your flowering career.
Whilst it is mandatory for Core Trainees to sign up to it, I encourage all our non-training SHOs to stump up and sign up. It demonstrates commitment, documents your CPD and its presence in your interview portfolio shows you've taken your career seriously.
So I met this week with some of the Core Trainees @ASPHFT to review their ISCPs for the first 2/12 of their posts. Here are Kamran and Daniel, both CT1s...
... and unsurprisingly at this early stage their portfolios seemed bereft of WBAs, tumbleweed drifting through the vast empty spaces of their 'evidence'... !!
It is a steep learning curve but once you get the hang of it, it becomes second nature to log everything you do.
Getting started
First up: open your ISCP to everyone. Meet early with your College Tutor who will set up your Global Objectives. This doesn't have to be face-to-face BUT I do like to clap eyes on everyone early on to get a handle on you and what you need and get your placements/supervisors validated.
Next: set up an early meeting with your Assigned Educational Supervisor to establish your Learning Agreement. This is the means by which topics are generated.
Topics
Ah, topics. "Linking topics" is a key indicator of progress at ARCP. Core Trainees should be selecting just the Core Training topics (2013). Don't forget this same ISCP is used for HST so there will be therefore topics appropriate for Higher Training. Core trainees are after the generic modules.
Work based assessments
WBAs: in @HE_KSS you need 40 per year, equally spread between CBDs, CEXs and DOPs. In the rush of excitement at being in theatre, of course you all clock up logbook figures (approx 200 needed) and generate PBAs but these are not wanted at Core ARCP: it's DOPs you need.
Every clinical interaction you have can be a WBA. Once you grasp that, it ceases to become a challenge to find the numbers. I tell my supervisees I expect to open my email every morning to be showered with the confetti of validation requests. I know it is possible, as their predecessors have done it. No biggie.
For CBDs and CEXs, on call and in clinics are fertile ground. Bear in mind half of each group of WBAs must be with a Consultant. T&O juniors must attend clinic once a week as part of their educational contract but I exhort all of you to try that, in your other specialities.
In T&O @ASPHFT all juniors are supernumerary (ie not even the registrars have their own template) which means there is time to train. Clinic is where you learn pattern recognition and decision making - every opportunity for case-based discussion.
Journal
The journal section is the ideal place to document (in real time) your reflective practice. Even if it's just a line about what went well or what tips you picked up, an interesting scenario etc. We must all demonstrate reflection for appraisal and revalidation. ISCP gives you somewhere reliable to store it. Try and use it as a work diary. I use it as College Tutor to document ad hoc meetings outwith the three set pieces.
Don't get fed up with the ISCP/portfolio process: it is easy to accuse it of being a tick box exercise but if you grasp the opportunity it offers with both hands it can be a fantastically useful tool to document your daily practice in one place.
Surgeon of the Week
Manish Kothari is this week's training hero, seen here with Sr Zenia Bolauro
Manish is a Breast Surgeon here @ASPHFT and one of my my most recent additions to the Surgical Faculty Group family. Currently a Clinical Supervisor he is going through accreditation to be an AES and is also a qualified Appraiser so has much to offer us as well as his enthusiasm and evident enjoyment of the job.
Paper of the Week
How could I pass up the chance of drawing your attention to this seminal work, "Are Surgeons Psychopaths?" In the Bulletin this week:
Forthcoming Attractions
This week I'm focussing on the CCrISP course: Care of the Critically Ill Surgical Patient. Doctors in CT1/2 and above can take this course and it is an essential requirement for HST eligibility. It is not open to Foundation Doctors.
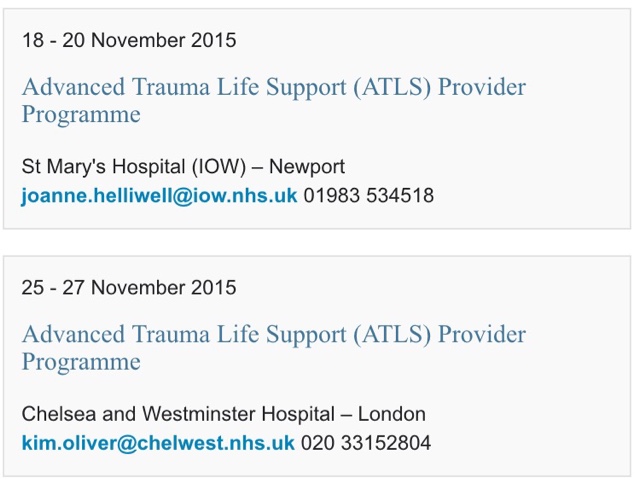
Looking at @RCSNews site, these are fewer in number and quickly booked up in comparison with other mandatory courses. Here are the more local ones that still have places:
Quick plug to the registrars for the @RNOHnhs Stanmore Shoulder Meeting: